He was a 31-year-old gay man, diagnosed with HIV in the 1980s, the terrifying early years of a deadly pandemic. He must have been terrified. But he was fortunate. For six years, unlike his friends and partners, he never fell sick. Eventually he donated some blood to a research project that was looking for long-term healthy survivors. His blood was processed and screened for antibodies, which were then tested against a variety of HIV strains. The testing revealed the secret of his long-term survival.
The volunteer’s name was never made public and his ultimate fate was not revealed, but we know that his blood contained unusually potent and versatile antibodies. His good fortune, along with his good deed, paved the way for antibody therapy, one of the most intriguing and long-running areas of HIV research.
Antibody therapy, which broadly encompasses both treatments and efforts to produce a vaccine, is essentially a refinement and strengthening of our natural defenses. According to Mario Stevenson, Director of the Institute of HIV/AIDS and Emerging Infectious Diseases at the University of Miami Miller Medical School, “All the efforts right now in vaccines and even in cure are focused on harnessing broadly neutralizing antibodies,” also known as bnAbs.
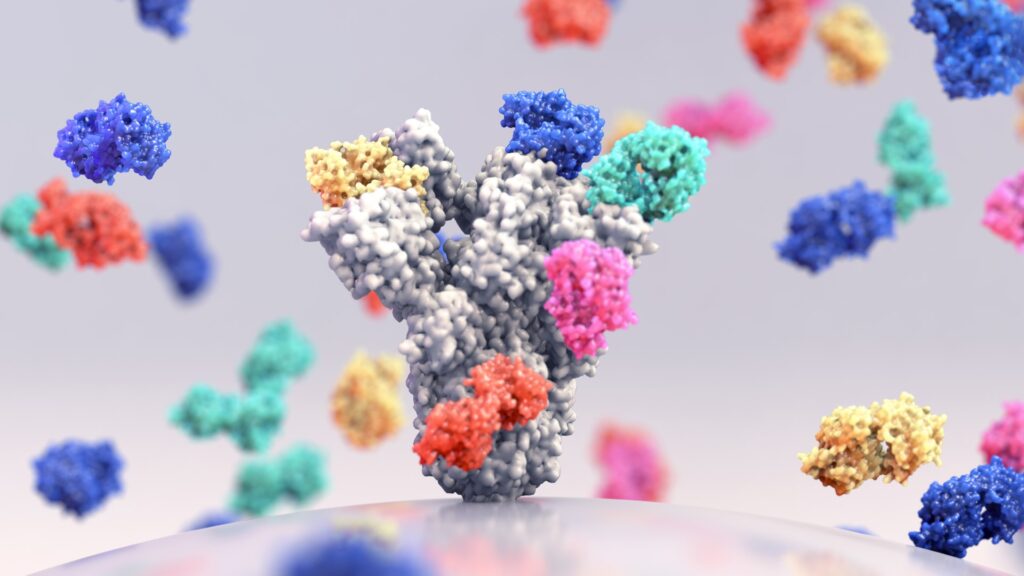
Antibodies are proteins that are generated naturally by the immune system as a response to antigens, which are substances, including bacteria and viruses, that provoke the body to produce a defensive immune response. Once in circulation, antibodies target specific proteins on the surface of these invaders, and either render them harmless or tag them for destruction.
The modern era of antibody treatments began in the mid-1980s, when the U.S. Food and Drug Administration approved the use of antibodies to prevent organ rejection syndrome in people undergoing kidney transplants. More than 100 monoclonal antibodies have been designated as drugs, making them one of the fastest-growing segments of the pharmaceutical industry. More than 30 monoclonal antibodies are approved by the FDA as treatments for cancer, heart disease and other ailments; millions of Americans with COVID-19 were successfully treated with monoclonal antibodies.
With HIV, the first super-potent antibodies to were discovered by a research team at the Scripps Research Institute, aided by that nameless volunteer. Since that first case, more than 200 HIV-specific broadly-neutralizing antibodies have been isolated from volunteers around the world. “We studied their [blood] serum,” says John Mascola, who retired in March as Director of the Vaccine Research Center at the National Institute of Allergy and Infectious Disease. “We found that the serum contained lots of different types of antibodies that could inactivate HIV.” For three decades, these antibodies have been a beacon of hope against HIV, which is one of the most formidable enemies in the realm of infectious disease.
Stevenson likens antibodies and antigens to competing fighters on a battlefield: “Most antibodies might recognize 30% of the enemy combatants, based on their uniform. The broadly neutralizing antibodies recognize over 90, 95 percent.” This makes them turbocharged versions of the body’s typical defenders.
“Monoclonal antibodies are a riff off of what the normal immune system does,” explains Mike Saag, Director of the University of Alabama at Birmingham Center for AIDS Research. The antibodies used for therapy are “monoclonal” because they’re clones of carefully selected antibodies that each target a specific site on the antigen. In modern antibody therapy, these clones are refined and multiplied, be even more effective attackers.
But HIV is a uniquely difficult target. The virus’ surface is cloaked in a dense coat of sugars, a kind of disguise, and is constantly shifting even underneath this cloak. The virus has a striking rate of mutation, calculated in one study to be faster than that of any living entity ever measured.
“Those protein surfaces, they change,” says Mascola, “So an antibody that sees one strain of HIV doesn’t necessarily see another one.”
This constant stream of mutations has been a major a roadblock to vaccine development and new treatments, but bnAbs offer a path forward. They are identified and selected in large part for their versatility, according to Saag, “so they don’t just work against one or two little variants, but against a number of variants.”
Starting in 2016, nearly 5,000 people have been given monoclonal antibodies in HIV clinical trials. The largest of these are known as the Antibody Mediated Prevention studies, or AMP. One AMP trial involved nearly two-thousand women in sub-Saharan Africa who were “behaviorally vulnerable” to HIV. The other recruited 2,700 men and transgender people who have sex with men, in the United States, Brazil, Peru and Switzerland. In both trials, volunteers received infusions of a monoclonal antibody to see if it would protect them, from infection,as with a vaccine.
The results left many disappointed. The monoclonal antibody, dubbed VRC01, reduced the odds only slightly that study volunteers would contract HIV during the year and a half that they were followed. Laboratory testing found that VRC01 successfully blocked strains of HIV for which it was well-matched – about a third of the HIV strains circulating – but the virus naturally mutated and evolved into strains that were resistant to VRC01.
“What we learned is that a single antibody can protect, but there are too many viruses out there that can evade one [single] antibody,” says Mascola. “That told us we need a cocktail of two or maybe three antibodies to cover all the diversity of HIV that exists.”
Stevenson says the results were predictable. “When you use one antibody alone, the virus makes mutations and is no longer sensitive to inhibition. We’re going to have to use a cocktail, in the same way we use cocktails of antiretrovirals.”
Indeed, the work with antibodies closely parallels the development of the antiretroviral medications that are the current gold standard for treating and preventing HIV. The major breakthrough came in the 1990s, when doctors recognized that using three antiviral medications simultaneously – often referred to as “combination therapy” or the “triple cocktail” – could successfully suppress the virus for long periods of time, even indefinitely.
For more than a decade, similar drug combinations have been FDA-approved as a means of preventing HIV infection in vulnerable people, and to prevent transmission by people who are HIV-positive. When taken as prescribed, so-called pre-exposure prophylaxis (PrEP) and Treatment as Prevention (TASP) are more than 99%t effective at blocking HIV transmission.
While some found the AMP results frustrating, others see the glass as half-full. One optimist is Larry Corey, a professor at Fred Hutchinson Cancer Center, who led the AMP trials and heads the HIV Vaccine Trials Network, an organization that coordinates HIV-related studies in 16 different countries.
“People are right when they say the one monoclonal antibody did not work as well [as antiretrovirals]. That’s true,” says Corey. “But it’s sort of like saying AZT [the first drug approved to treat HIV] didn’t work as well as triple combination therapy. That’s history. We did the AMP trial on purpose with one antibody, because we wanted to see what would happen. And we learned exactly what we wanted to learn.”
Among the lessons: monoclonal antibodies are safe, and show a proven ability to fight back against HIV in real patients. To Mascola, it was a successful proof of concept. “The initial studies told us that we need a little bit better antibodies than we have right now, but I think there’s a strong sense that it’s very possible. It’s more of an engineering problem than a scientific, conceptual problem,” he says.
Mascola and some others believe that monoclonal antibodies could ultimately have a supporting role in maintaining long-term suppression of the virus. HIV-positive patients might receive antibodies in tandem with long-acting antiretrovirals that are given every few weeks, rather than as a daily pill. “We could augment the antiretroviral drugs with an antibody,” suggests Mascola, “so that if the virus tries to escape the drug, the antibody will pick it up. If the virus tries to escape the antibody, the drug will pick it up.”
The challenges of finding a treatment for HIV aren’t unique. All viruses adapt their own defenses. Monoclonal antibody therapies were highly effective during the early waves of COVID-19, but not against more recent variants.
With HIV, major hurdles remain. For one thing, monoclonal antibodies are generally more expensive to produce than the current crop of antiretrovirals. A more basic hurdle is that the body degrades monoclonal antibodies over time, so that regular infusions are required to sustain protective levels.
Some researchers are working to engineer antibodies to last months rather than weeks, but a more ambitious solution would be inducing the body to produce, on its own, specific antibodies needed to fight HIV. “If we can find a way to train the B cells within our bodies to produce those neutralizing antibodies, that could be a winner in terms of a vaccine,” Saag says.
That basic approach is being explored in the lab of Ronald Desrosier at the University of Miami Miller School of Medicine. In a remarkable experiment, Desrosiers and his colleagues used a novel method to apparently cure three rhesus monkeys of AIDS virus infection. The team gave infected monkeys an intramuscular injection of adeno-associated virus (AAV), a virus engineered with genetic instructions to produce three antibodies designed to attack the AIDS-like virus. Within days of the first injection, the monkeys were functionally cured of SIV infection. One of the animals has remained virally suppressed for more than five years.
“Once you get AAV into those cells, they will produce those [antibody] proteins forever,” explains Derosiers. “Unfortunately, it only works in a small proportion.” While three rhesus monkeys were functionally cured by the experimental treatment, most animals who received the injection developed what are known as “anti-drug antibodies” or ADAs. In other words, the immune system produced antibodies to AAV itself, blocking the vector from ensconcing itself in muscle tissue and preventing it from producing the antibodies being made by the AAV, negating their benefit. Desrosiers’ lab is looking for a way around the problem, but there’s no easy fix.
Corey says it’s important to continue the work, even if the ultimate path is unclear. After all, successful treatments for COVID-19, Ebola were only made possible by previous, groundbreaking work on HIV. “That was really a gift that HIV developed, this quest to develop human monoclonal antibodies. Where did they attach on the virus? And could we make a vaccine at that point of attachment? That technology led to the isolation of human antibodies. And then that became, ‘Oh, we can do this for other diseases.’”
The path to breakthrough treatments is often winding, long and unpredictable. For many patients, HIV has become a chronic, manageable condition but it remains, for the most part, incurable.
This reporting was supported by HHMI Tangled Bank Studios